Spinous Process Fracture
What is a Spinous Process Fracture?
A spinous process fracture is a stable injury that can be severely painful but doesn’t pose any danger to the spinal cord or nerves within and around it. A fracture in the spinous process, while not posing any significant threat, is a more serious injury that requires medical attention and treatment. There are several ways to fracture the spinous processes and multiple treatment options that range from conservative approaches to spine surgery.
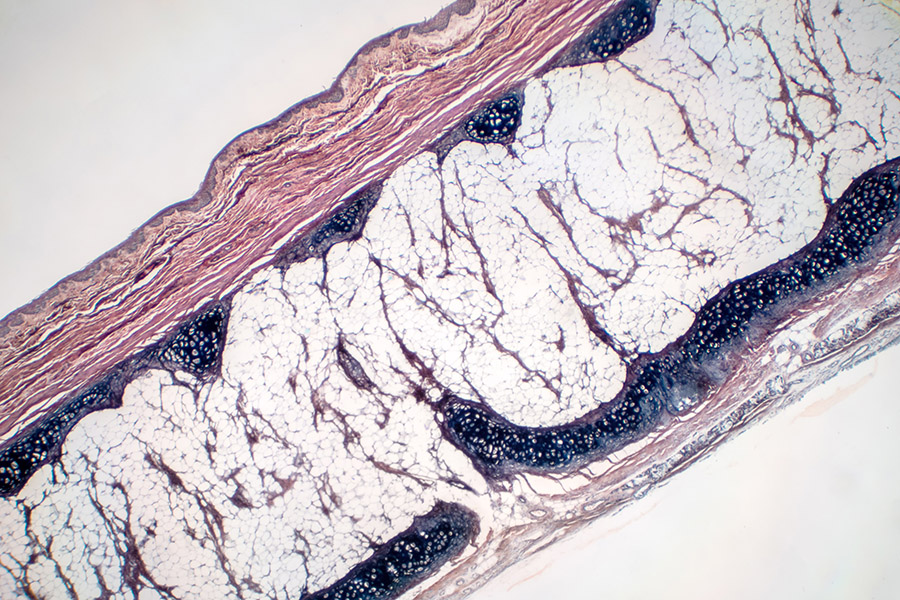
What is the Spinous Process and its Function?
The spinous process is a bony projection off the back part, or posterior, of each vertebra in the spine. When you run your hand down the middle of a person’s back, you can feel a series of bumps which are the spinous processes.
Each vertebra has several important bony projections:
- Spinous process: Projects towards the back from the junction of the two laminae.
- Transverse processes: Project toward the sides and slightly back from the junctions of the pedicles and laminae. There are two transverse processes for each vertebra, one on each side.
- Superior and inferior articular processes: These are pairs of bony bumps that connect with the bones above and below them, creating joints that let the spine move and stay stable.
The spinous processes serve several functions:
- Muscle attachment: Several muscles and ligaments of the back and spine attach to the spinous processes.
- Protection: They add an extra layer of protection to the spinal cord and nerves.
- Leverage: They provide leverage for certain movements of the spine.
Symptoms & Causes of the Fracture
Symptoms of spinous process fractures depend on the location of the fracture in the back but often include:
- Muscle weakness
- Trouble moving the body where the fracture occurred
- Loss of bladder or bowel control
- A dull pain that can last for several days or weeks
- Swollen, bruised, numb, or tingling skin over the area where the fracture occurred
- A sudden, sharp, stabbing pain that can be more severe when moving or breathing
A spinous process fracture can develop for several reasons and there are risk factors that increase the likelihood of one occurring. Risks include older age, osteoporosis or low muscle mass, and contact sports or sports where twisting the body is common. Causes of a fractured spinous process include:
- Trauma: direct blows or injuries to the back, such as in a car accident or fall
- Repetitive strain: overuse can lead to stress fractures of the spinous process
Diagnosis & Treatment for Spinous Process Fracture
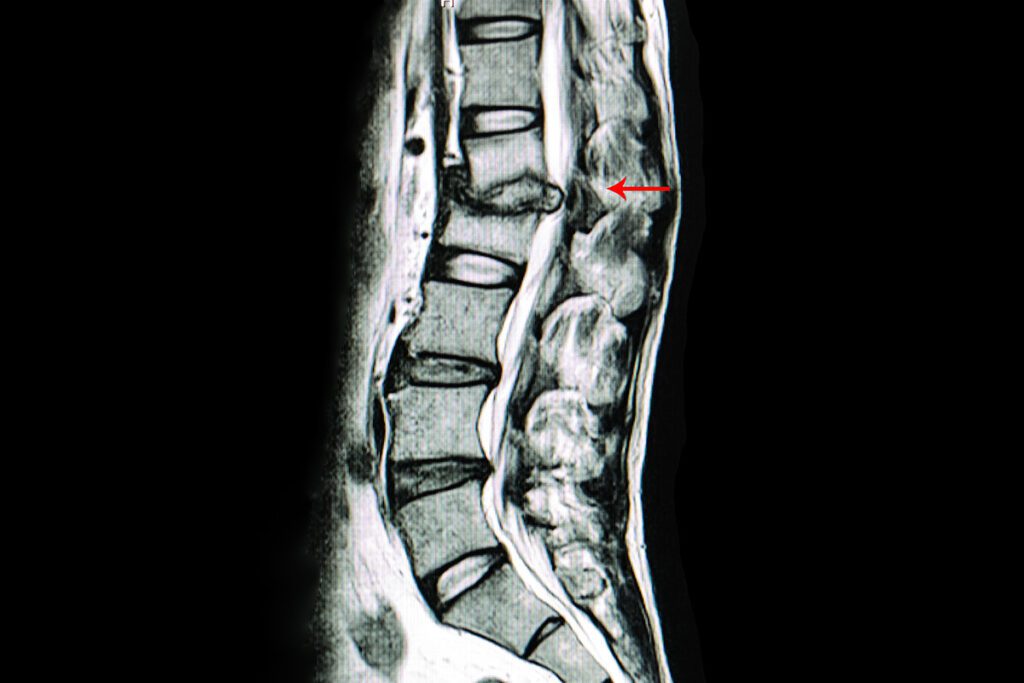
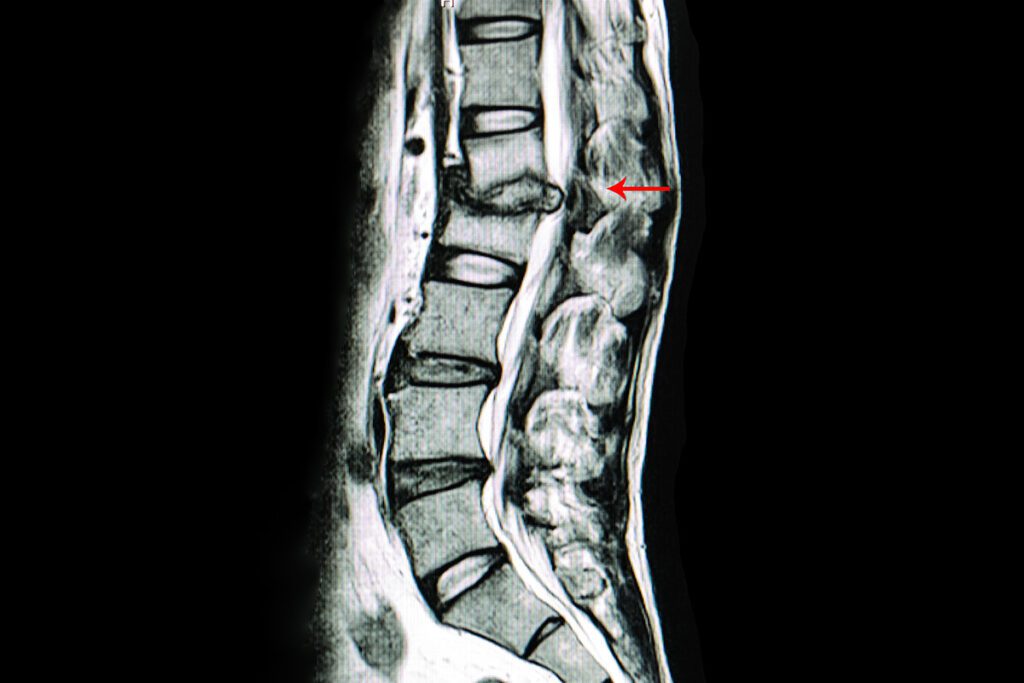
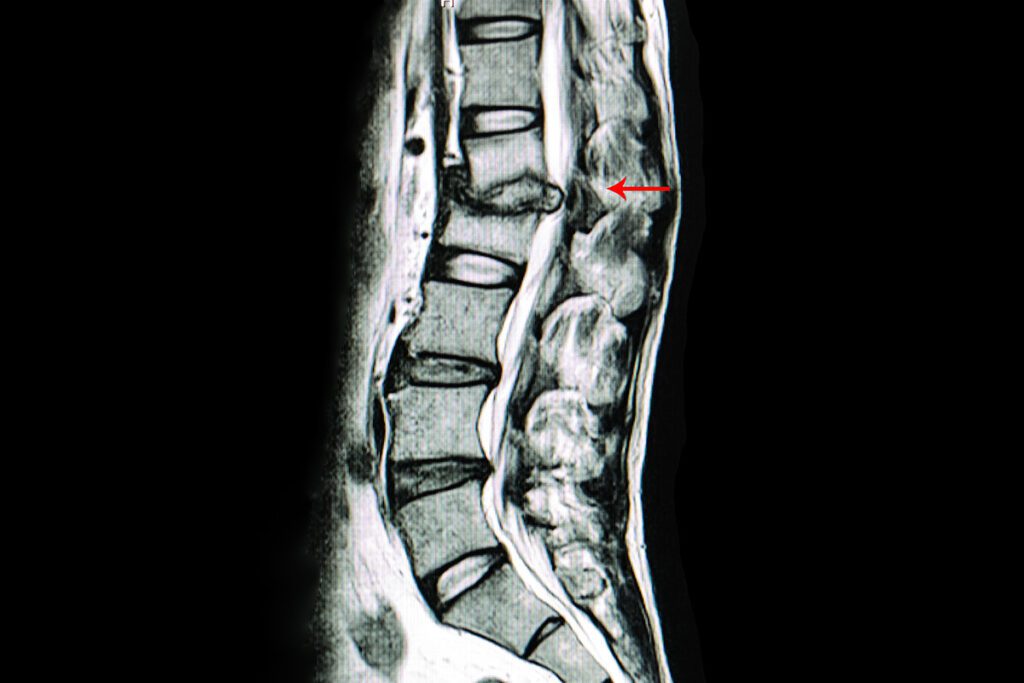
To diagnose a spinous process fracture, a healthcare provider will perform a physical exam and ask questions about the symptoms their patient is experiencing, what happened that caused the symptoms, and order imaging tests to confirm suspicious of the fracture, such as:
- X-rays: to show the fracture and any muscles or tissues that may have been injured
- MRI or CT Scan: if a fracture doesn’t appear on the X-ray, a doctor may double-check using either of these imaging tests to make sure there is no fracture present.
Treating the fracture depends on the severity and can be nonsurgical or require an operation:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Such as ibuprofen (Advil, Motrin) or naproxen (Aleve). These can help reduce pain and inflammation.
- Acetaminophen (Tylenol): Can be used for pain relief.
- Prescription pain medications: For severe pain, opioids might be prescribed, but they are typically used for a short duration due to concerns about addiction and side effects.
These can be prescribed if there are muscle spasms associated with the injury.
If the fracture is due to weakened bones from osteoporosis, medications to treat osteoporosis might be recommended.
Like alendronate (Fosamax) or risedronate (Actonel), these are used to prevent and treat osteoporosis.
In some cases, medications like teriparatide (Forteo) that help stimulate bone growth might be prescribed.
To keep a person from moving the area and ensure proper support to allow the fracture to heal.
If the fracture is severe, has associated injuries, isn't healing properly on its own, or is causing significant pain that isn't relieved with medication, surgery may be recommended. Either a kyphoplasty or vertebroplasty would be likely depending on the severity of the fracture.
Spine Doctors
Request an Appointment
Resources



All About Compression Fractures: Causes, Symptoms, and Treatment Options
A vertebral compression fracture is where adjacent vertebral bones are compacted against each other. Osteoporosis, traumatic injuries, or tumors can cause this fracture. Continue below to learn more about the causes, symptoms, and treatment options for compression fractures. What Are Compression Fractures? Compression fracture is a type of fracture in
Disc Protrusion
Disc protrusion is a common type of spinal disc deterioration that causes neck and back pain, but can be referred to in other ways. This type of spinal condition often comes with age and if felt, can cause someone alarm; but, it’s a common type of spinal condition that can